
Revision Total Hip Replacement
Total hip replacement is a very successful operation and only a small percentage will fail and require a revision hip replacement. It is a common myth that total hip replacements will often need to be revised after ten to fifteen years.
The Australian Orthopaedic Association manages the Australian Joint Replacement Registry and has done so for fourteen years. This registry collects data on all joint replacements performed in Australia and is regarded as one of the best registries of its kind in the world. This registry provides two benefits to patients.
- It identifies prostheses that have a high revision rate and surgeons make choices about the prostheses they use based on this information. This has led to a decrease in revision rate as surgeons use the available data to choose better performing prostheses.
- The data collected by the registry has demonstrated that only 5% of hip replacements have required revision at ten years post operatively. Fourteen years after surgery 7.8% of hip replacements require revision.
Causes of Failure of Hip Replacement
Loosening / Osteolysis
This is the most common cause of joint replacement failure. In some cases a high rate of wear of the bearing surfaces occurs and the wear debris from the joint replacement surfaces can induce an immune response in the surrounding tissues. This immune response causes damage to the surrounding bone and soft tissues. If it damages the bone excessively the prosthesis (femoral or acetabular component or both) may become loose. This may cause:
- a limp
- shortening of the leg
- increasing pain during activity
The incidence of loosening has been reduced over the last fifteen years due to improvements in the prostheses used in joint replacement surgery.
Infection
Infection can occur either soon after surgery or some months or years later. It is caused by a bacteria lodging around the prosthesis at the time of surgery but may not become obvious for weeks or even months after the operation. However most patients with a deep infection have more pain than normal immediately after surgery.
Late infections can occur many years after surgery and are usually blood born in nature. This means that infections elsewhere in the body (for example urinary tract infections and dental abscesses) can be carried by the blood stream into the prosthetic hip joint.
Sometimes infection can be successfully treated by washing out the joint several times under anaesthetic. This is done in conjunction with the administration of high-powered intravenous antibiotics.
When this is not successful a two-stage procedure is required. Firstly the original prosthesis and any surrounding infected tissue are removed. It is usual to insert an antibiotic covered spacer to maintain the length of the limb while the infection is brought under control.
Once there is evidence that the infection has been eradicated a second stage revision hip replacement is performed. This will usually be done at least three months later.
Dislocation
Dislocation of a prosthetic hip occurs when the prosthetic femoral head slides out of the acetabular cup. The greatest risk of this complication is in the first six weeks after hip replacement surgery. Dislocation causes severe pain and requires urgent ambulance transfer to the emergency department where the dislocation can usually be reduced under sedation. In the majority of cases dislocation does not occur again. However if there are repeated instances of dislocation then a revision hip replacement will be required.
Fracture
As patients become elderly and frail they may become prone to repeated falls. A fracture of the femur (or occasionally the acetabulum) may occur close to the prosthesis. On some occasions it can be successfully managed with internal fixation with plates and wires. Sometimes it is best to revise the joint to a larger and longer femoral prosthesis.
Preoperative Consultation
After taking a history and a thorough examination the surgeon will discuss non-operative and surgical options with the patient. Revision hip replacement is a major procedure and sometimes can be quite complex. The surgeon may therefore recommend a further consultation prior to performing revision hip replacement.
Further tests may be ordered in addition to plain x-rays and these will include:
- Blood tests to rule out low-grade infection.
- Bone scan – this involves injecting a small amount of radioactive dye into a vein before images are taken. Imaging will be done five minutes later and again after three hours. This test can be helpful in diagnosing loosening and or infection of the prosthesis.
- CT scanning. This is done to assess the degree of bone damage. It can also be used to make a customised revision implant when the bone damage is extensive.
After the decision has been made to proceed with revision hip replacement a consultation with a specialist physician may be arranged in order to optimise the patient’s medical condition prior to surgery.
Preoperative Patient Education
At the time of the consultation the patient will be given a full explanation of what is involved in the joint replacement procedure, expected recovery period and eventual outcome.
If there are any concerns or questions that arise for patients after the consultation, the staff at KOG welcome calls from patients to clarify any of these issues. If the issues require further explanation a further consultation with the surgeon is encouraged.
The patient will be asked to attend a pre-operative education session at Knox Private Hospital. This is conducted by experienced nurses and physiotherapists. If the patient is aware of what is going to happen to them, they are usually less fearful and anxious about the procedure. This increased knowledge has been shown to reduce postoperative pain and make the recovery less stressful.
Patient Stay in Hospital
The patient will be admitted to hospital on the evening prior to surgery. Pre-operative investigations will be carried out including blood tests and an ECG.
The procedure will be carried out under a spinal and/or general anaesthetic. A urinary catheter will be inserted to monitor urine flow during and after the procedure.
Post-operative recovery
For prolonged or more complex procedures the patient may go to the Intensive Care Unit for monitoring post operatively. In most cases the patient will be mobilised out of bed the day following surgery. Due to the complexity of surgery the patient will have protected weight bearing for six weeks post operatively. Many patients will be transferred after four to five days to a rehabilitation hospital (Donvale or Vic Rehabilitation).
The Operative Procedure
The procedure may take between one and four hours depending on the complexity of the operation. A blood cell saver may be used. This device allows blood to be retrieved during the operation and transfused back into the patient. This minimises the amount of donor blood needed for transfusion.
The nature and complexity of the surgery will vary and depend upon the causes of the failure of the original hip replacement. The surgical options include the following:
- Simple exchange of modular femoral head and acetabular liner. This straightforward procedure would be indicated where there is excessive wear of the bearing surfaces but the remaining prosthesis remains well fixed to bone.
- Removal of acetabular and/or femoral component. This can sometimes be simple and at other times very challenging. In order to remove the femoral component an extended trochanteric osteotomy may be required. At the end of the procedure this will need to be held with wires and/or plate. See Figure 3
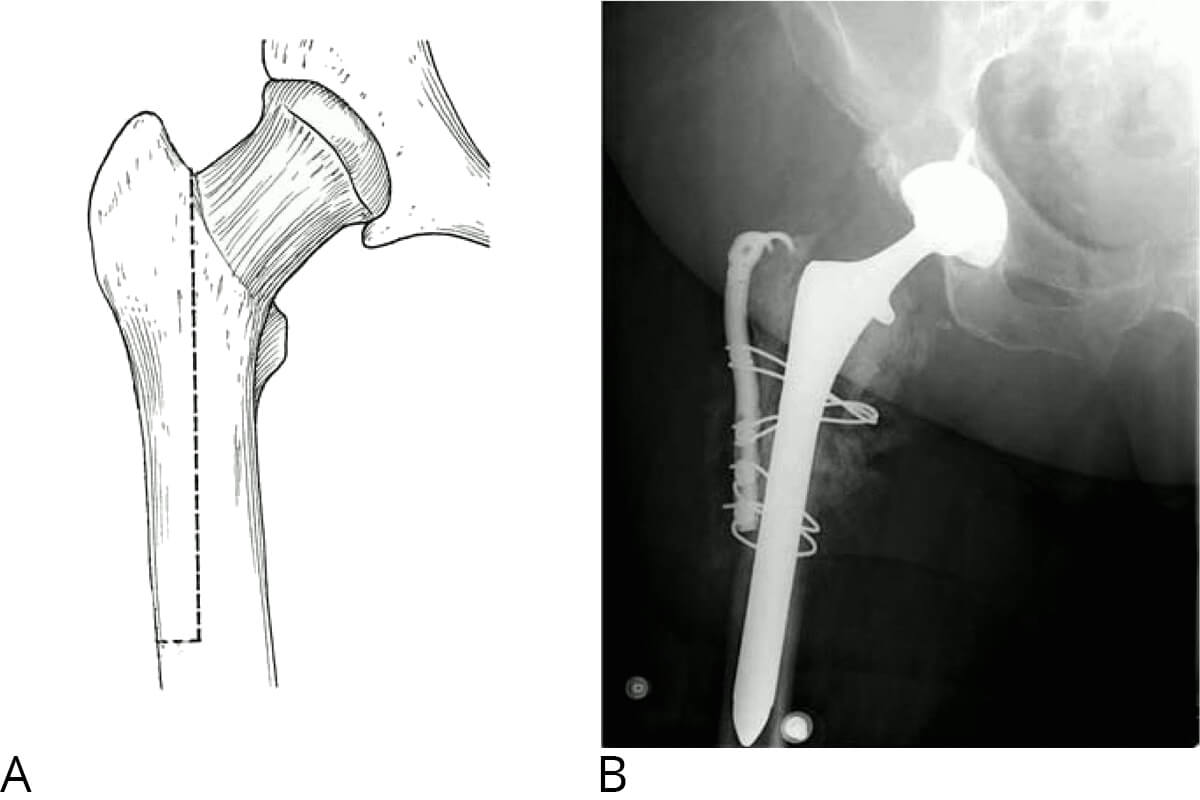
Fig 3: Extended Trochanteric osteotomy with post operative X-ray.
- Insertion of a new prosthesis. This will usually involve inserting a larger and longer prosthesis than the original. The femoral revision prosthesis consists of several components and is made of titanium. The acetabular component also has several components and may have titanium augments that fill the space where the bone has been damaged.
- Bone graft. Allograft is often used to make up for the damaged bone. It is procured from a bone bank and consists of bone taken from a bank that stores bone from organ donors. This bone is tested for communicable diseases (in a similar way to the management of blood donation) prior to insertion.
- A variety of bearing surfaces may be inserted. These are designed in a particular way to minimise the risk of postoperative dislocation.
- For infected cases:
- Stage 1 involves removal of existing prosthesis and removal of all infected soft tissue. Usually a cement spacer impregnated with antibiotics is inserted.
- Stage 2 involves removal of antibiotic spacer and insertion of revision prosthesis.

Fig 4: Previous infected THR treated with antibiotic spacer and large defect in acetabulum.
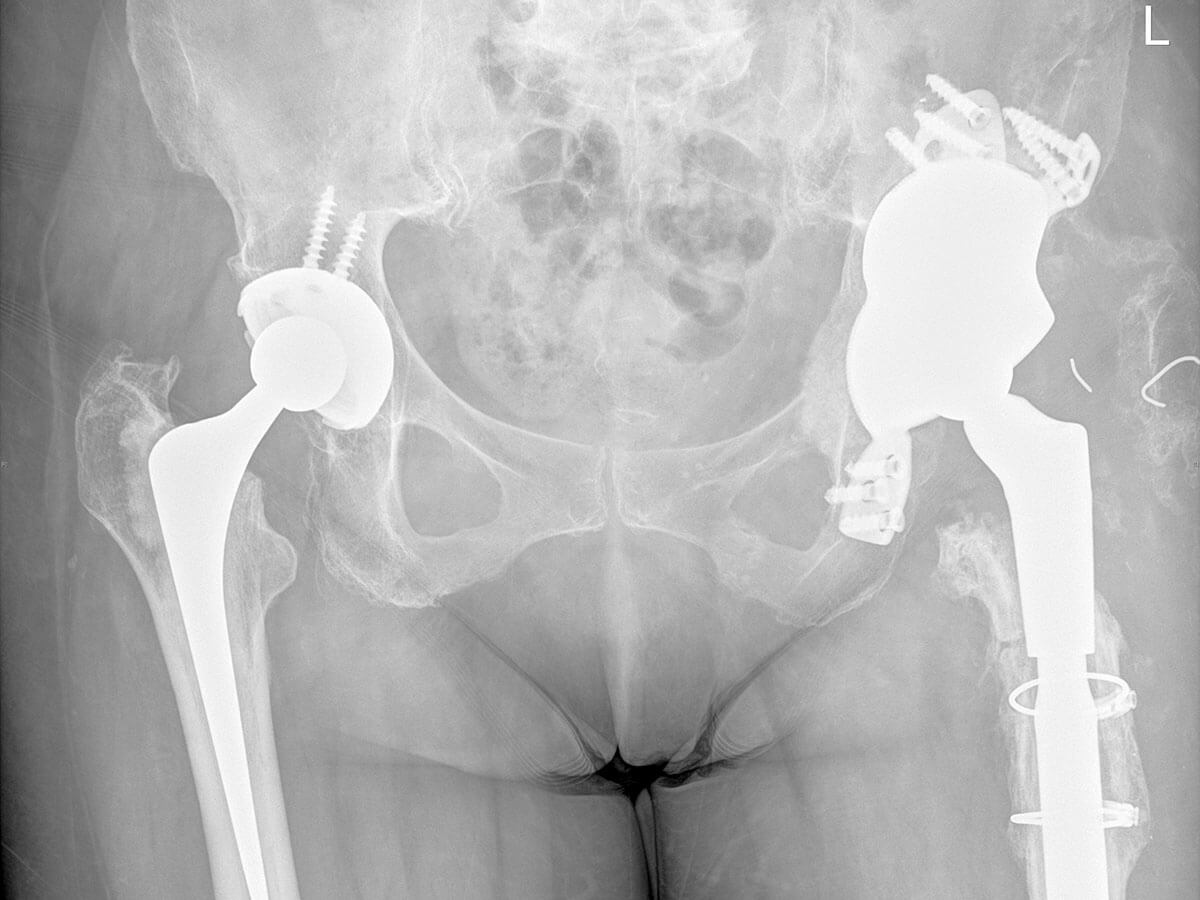
Fig 5: X-Ray after 2nd stage revision THR with modular femoral stem and custom built acetabulum.
Systemic Complications
These can occur in the postoperative period. Revision hip replacement surgery is a major stress on the body, and if there are pre-existing medical conditions, the following complications may occur:
- Heart attack
- Stroke
- Pneumonia
- Short Term Confusion
Local Complications
Blood Clots (The medical term for these is Deep Venous Thrombosis)
Measures are taken to minimise this complication, including the wearing of stockings and foot pumps to improve blood flow in the legs. Aspirin or Heparin is used to thin the blood. In addition, patients are mobilised on the day of the operation. Whilst these measures significantly reduce the risk of deep venous thrombosis this condition can still occasionally occur, sometimes the blood clots can travel to the lungs and cause a pulmonary embolus that can have quite serious consequences including death.
Infection
Superficial infection is an uncommon complication that usually responds well to antibiotics. A deeper infection is much less common but can have serious long-term consequences. It sometimes requires further surgery and prolonged high-powered antibiotics.
Dislocation
Sometimes the ball and socket joint can dislocate which would cause acute pain and the inability to walk. The hip can usually be put back in place by manipulation without the need for open surgery. It is more common in the first few weeks postoperatively and there are precautions that can be taken to minimise this complication.
The risk of this complication is greater in revision hip surgery.
Leg Length Discrepancy
In many cases the leg will be shorter prior to revision hip surgery. Every endeavor is made to restore the legs to equal leg length.
Nerve Injury
This is an uncommon complication of revision hip replacement surgery. However it is more common in revision hip surgery than in primary hip replacement surgery. It can lead to weakness or altered feeling in the foot and ankle. It usually improves but can be permanent.
